The Itch that Rashes!
Atopic dermatitis, commonly called eczema, is ruefully known as the “itch that rashes.” Patients with this skin condition suffer from itchy, inflamed skin. The itching, which can be intense and miserable, often develops first. Though scratching momentarily relieves the itch, it also causes the development of inflammation or rash. The ensuing “itch-scratch-rash” cycle only worsens the dryness, itchiness, and overall appearance of the skin.
Healthy skin acts as a barrier to keep unwanted substances (such as allergens, irritants, and toxins) out of the body and keep good things in the body (such as moisture). When this barrier is not working properly, substances penetrate the skin and trigger an immune response. Breakdown in the skin barrier also leads to moisture loss in the skin. The end result is dry, itchy, inflamed areas of skin. Recent studies point to a defect in the skin barrier protein called filaggrin as a factor in disease development in some patients.
Atopic dermatitis often begins in childhood, usually infancy, and is more common in individuals who have hay fever or asthma, or have family members who do. The condition falls into a category of disease called “atopic,” which also includes food allergy, hay fever, and asthma. These diseases may develop one after the other over a period of years; this is known as the “atopic march.” Recognizing this progression can be helpful and lead to earlier diagnosis and treatment.
Genetics play a role in the development of atopic diseases, although the exact way they pass from parent to child is not yet known. This means that a person is more likely to have atopic dermatitis, allergies, or asthma if other family members have ever had these diseases before. If one parent has an atopic disease, the likelihood that their child will develop one or more atopic diseases is approximately 50%.
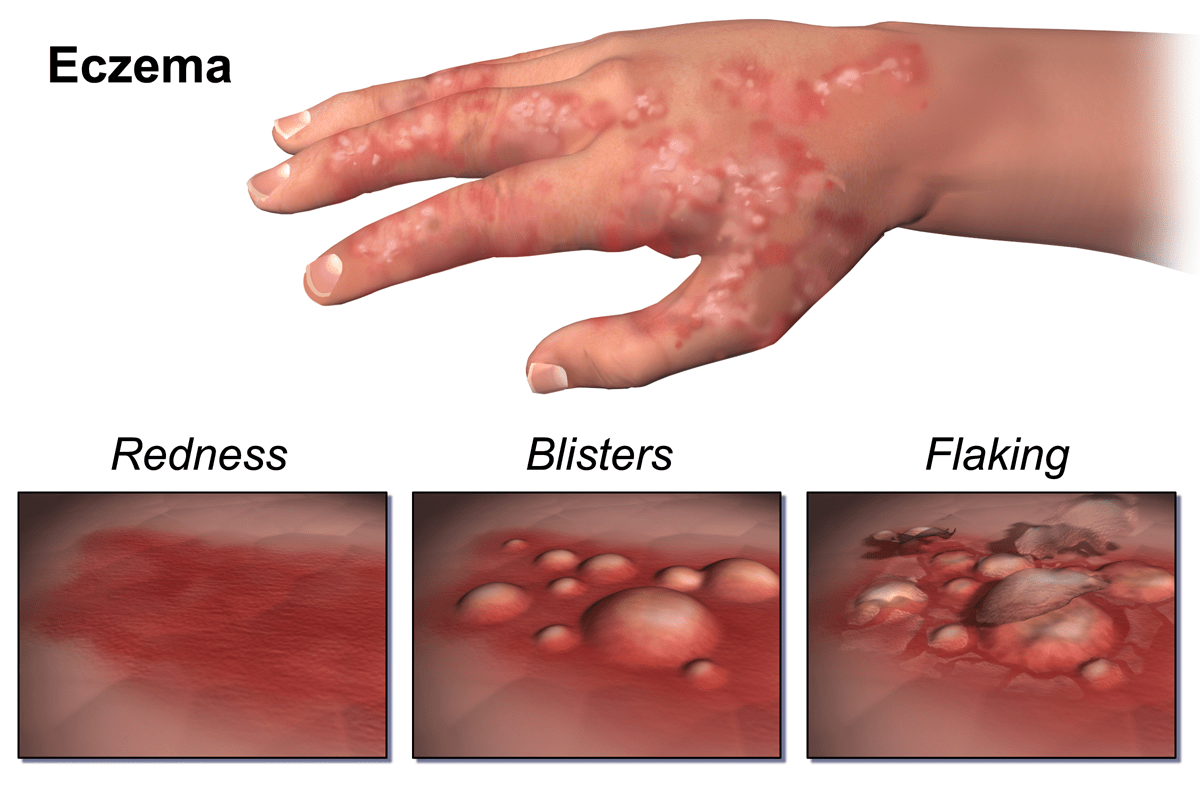
Although eczema can affect any area of the skin, the location and appearance of a rash often vary with age. In early infancy, eczema is the most prominent on one’s face and head with a red, weepy rash. After six months of age, the outside of the elbows and knees may worsen, along with other areas than can be easily reached for scratching.
In older children and adults, the creases of elbows, knees, wrists, and ankles are more common, as well as around the eyes. The rash will likely have a dry appearance, yet a variety of presentations are possible, including scaling, bumps, thickening, redness, and cracking. Some individuals suffer with specific hand eczema.
In more severe cases, atopic dermatitis can be body-wide and cause crusting. Secondary skin infections may develop, requiring the use of antibiotics to half the cycle. Although patients with atopic dermatitis often have higher levels of staph bacteria on the skin, the condition is not contagious.
Atopic dermatitis can improve with age. However, the disease tends to be episodic, waxing and waning. Specific triggers for exacerbations vary from person to person, but include dry winter air, stress, heat and sweat in the summer, exposure to food allergens, airborne allergens, contact allergens, cold viruses and other infections.
An important part of managing atopic dermatitis, and the relentless itch-rash cycle, is proactive skin care to keep the skin barrier intact. Dry skin is brittle, while moist skin is flexible; therefore, lubrication is of primary importance. Moisturizers and barrier ointments work best when applied to damp skin, such as immediately after bathing. Excessive scrubbing and toweling should be avoided. Lotions containing alcohol must be avoided, as they can dry out the skin.
A combination of prescription medications, over-the-counter medications, and topical therapies are used in the treatment of atopic dermatitis. Specific allergens may be triggering exacerbations. These allergens can be identified by an allergist. An allergist can also identify the skin care routine appropriate for your specific situation. Although other medical specialities, such as dermatology, also see eczema patients, an allergist is able to test for possible allergen triggers. A referral is not needed to see an allergist unless it’s required by insurance. With regular care, the itch that rashes can become the itch that vanishes!
Further information and resources can be found at your local allergist’s office, The American Academy of Allergy, Asthma, and Immunology, or The National Eczema Association.
Check out our clinical research trials on eczema and atopic dermatitis; we may have the solution you have been waiting for!
Written by Dana Dalbak, PA-C.

Dana Dalbak, PA-C
Dana Dalbak, PA-C, is a certified Physician Assistant, graduating with a Master’s Degree from Central Michigan University. After placing in the tenth percentile on the National Physician Assistant Certification Exam, she traveled to Gambia, West Africa to complete the rest of her training. Upon practicing family medicine for five years in an underserved part of Michigan, where she has worked with Dr. Siri in Allergy and Asthma specialty care since 2007. She has been a wonderful part of the MASA family since its establishment in 2013.
View Dana’s full biography here.


